Brachycephaly is a common head deformity in infants, characterized by a short, wide, or flattened back of the skull. While often harmless, it can sometimes indicate underlying cranial conditions that may need medical attention. Understanding its causes, how it is diagnosed, and available treatment options can help parents ensure healthy skull and brain development in their baby.
What is Brachycephaly?
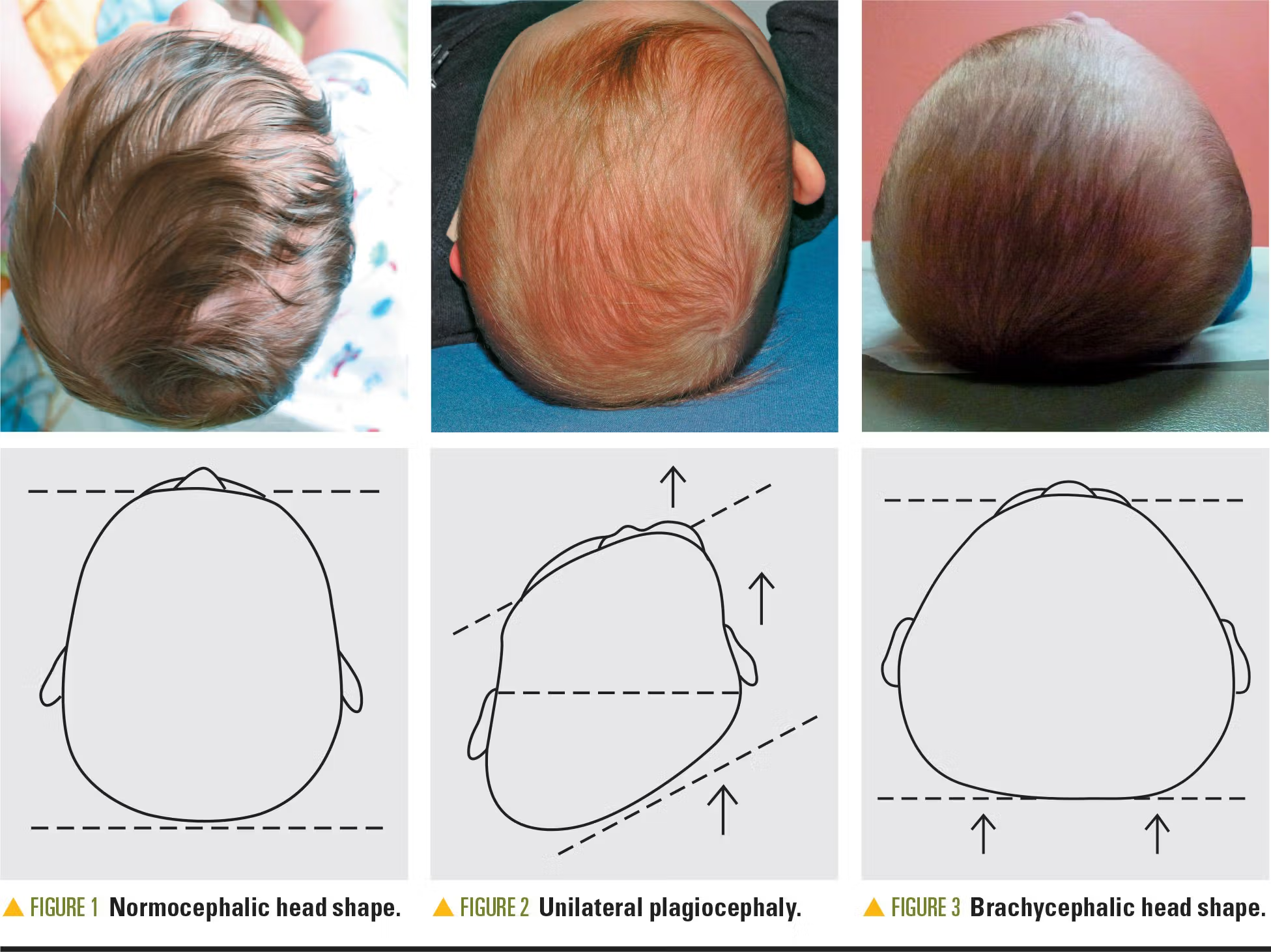
Brachycephaly is a type of positional or structural skull deformity where the back of the head appears flattened, giving the head a wider and shorter appearance. Brachycephaly typically involves flattening across the back of the head (often symmetric). If flattening is mostly on one side, it may be plagiocephaly.
- Positional Brachycephaly: Caused by external pressure, often due to prolonged time spent lying on the back.
- Craniosynostotic Brachycephaly: Caused by premature fusion of the coronal sutures, requiring medical evaluation and possibly surgery.
Causes of Brachycephaly
Brachycephaly can develop due to positional factors or cranial suture abnormalities:
1. Positional Factors
- Spending long periods lying on the back (sleep position)
- Limited tummy time during infancy
- Premature birth with softer skull bones
- Multiple births, such as twins, which reduce space in the womb
2. Craniosynostosis (Premature Suture Fusion)
- Coronal sutures fuse too early
- Leads to abnormal skull growth
- May increase pressure inside the skull
- Can affect facial symmetry
Signs and Symptoms of Brachycephaly
Parents should watch for the following:
- Flattened area at the back of the head
- Wider than normal head shape
- Head appears short from front to back
- Ears may appear pushed forward
- Positional brachycephaly is not believed to cause brain injury. If developmental concerns exist, they may be related to associated factors (such as torticollis) or other underlying conditions and should be evaluated.
Early detection is important for better treatment outcomes.
How is Brachycephaly Diagnosed?
Diagnosis usually involves a physical exam and imaging studies:
1. Physical Examination
- Pediatrician evaluates skull shape, symmetry, and growth
- Measures head circumference and width
- Most cases of brachycephaly are diagnosed clinically through physical examination. Imaging is typically reserved for cases where craniosynostosis is suspected. When imaging is needed, CT scans are the most common confirmatory study.
3. Medical History
- Birth history, sleep patterns, and family history of cranial deformities
A correct diagnosis is essential to determine whether the brachycephaly is positional or craniosynostotic, which impacts treatment decisions.
Treatment Options for Brachycephaly
Treatment depends on the severity, type, and age of the baby.
1. Repositioning Therapy
- Recommended for mild, positional cases
- Encourages the baby to spend time on their tummy while awake
- Change head position when sleeping or feeding
- Usually effective within months if started early
2. Helmet Therapy
- Custom-molded cranial helmets
- Guides skull growth over time
- Typically used for moderate to severe positional brachycephaly
- Most effective when started between 4–6 months of age
3. Craniofacial Surgery
- Needed in cases of craniosynostosis related brachycephaly
- Surgery corrects premature suture fusion
- Restores normal head shape
- Prevents increased intracranial pressure and developmental complications
Benefits of Early Treatment
Early intervention can help:
- Improve skull symmetry and appearance
- Reduce potential developmental or neurological risks
- Minimize need for invasive procedures
- Improve long-term cosmetic and functional outcomes
Preventing Positional Brachycephaly
Parents can reduce the risk of brachycephaly with simple strategies:
- Provide tummy time while the baby is awake
- Vary sleeping positions safely (following safe sleep guidelines)
- Limit time spent in car seats, swings, or bouncers
- Encourage interaction and movement that changes head pressure
Long-Term Outlook
Most babies with positional brachycephaly have normal development and experience improved head shape with early intervention. Children with craniosynostosis who receive timely surgical treatment also have excellent long-term outcomes, including healthy brain development and balanced facial growth.
When to See a Specialist
Consult a pediatrician or craniofacial specialist if:
- Head shape appears unusually flat or asymmetrical
- Flattening does not improve with repositioning
- Ears, forehead, or face appear uneven
- Signs of craniosynostosis or developmental delay
Early evaluation allows the most effective treatment and better results.
Conclusion
Brachycephaly is a common head deformity in infants that can range from mild positional flattening to more serious cranial suture fusion. With early diagnosis, repositioning, helmet therapy, or craniofacial surgery, most babies achieve normal skull shape and healthy development. Awareness, regular monitoring, and timely consultation with specialists are key to successful outcomes.
Schedule a Pediatric Craniofacial Consultation
NJ Craniofacial Center Providing expert, compassionate craniofacial care for children across New Jersey.